The Daily Observer London Desk: Reporter- John Furner
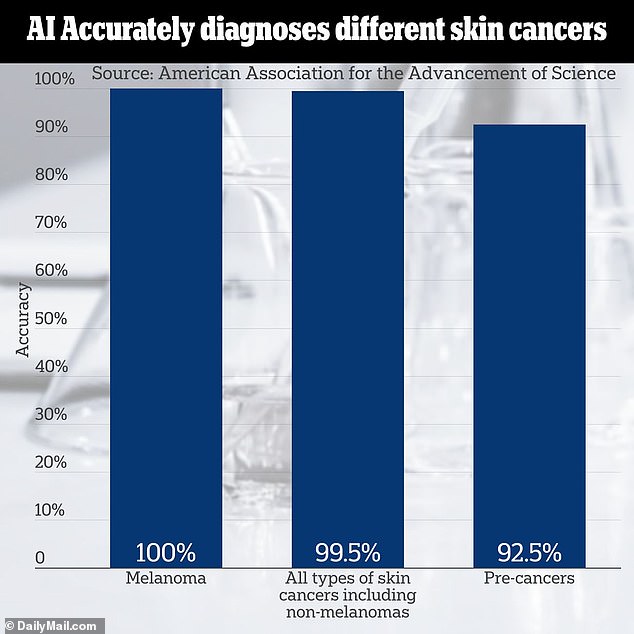
Artificial intelligence software can now detect signs of the most deadly type of skin cancer with 100 percent accuracy, potentially catching some of the most fatal cases in earlier stages when they have a better chance of being treated.
Dermatologists debuted the third generation of their AI system, which was able to identify all 59 cases of melanoma, which typically appears as an irregularly shaped mole of different colors.
And of 190 cases of any skin cancer, including melanoma and less fatal types, the AI software only missed one.
Melanoma is the most fatal of skin cancers, killing more than 57,000 people worldwide in 2020 alone. However, non-melanoma cancers including squamous cell carcinoma and basal cell carcinoma, which are far less deadly but much more common, account for more deaths worldwide.
Artificial intelligence has increasingly become a point of controversy in healthcare due to privacy and ethics concerns, but medical researchers are embracing it as a possible means to streamline administrative duties and speed up the time to diagnosis to give patients the best chance of survival.
The researchers behind the study had been fine-tuning the technology for three years before hitting peak accuracy for melanoma, and near total accuracy for other skin cancer diagnoses

Skin cancer is the most common type of cancer in the US with an estimated one in five expected to develop it in their lifetime
Dermatologists from the UK have been fine-tuning the AI cancer detection software for the past three years, and have ‘trained’ IT using patient data from consultations with doctors and images of their cancers.
More than 22,350 people in the UK over two and a half years tested the AI’s ability to spot their cancers and pre-cancerous growths.
Dermatologists and medical photographers loaded the system with patient data including photos of cancers to ‘teach’ it what to look for.
The latest version of the software was fed more than 1,000 patient consultations to improve diagnostic accuracy.
The AI then sorted through the data to distinguish between non-cancerous lesions and possible cancers, or ‘malignancies’. Dermatologists then reviewed the AI software’s diagnoses.
It correctly diagnosed all 59 cases of melanoma, as well as 99.5 percent of all skin cancers overall, including melanoma and nonmelanoma cancers, a stark improvement from the first version’s level of accuracy of 83.8 percent.
It also correctly spotted pre-cancerous growths on skin nearly 93 percent of the time, 38 percentage points higher in accuracy compared to the first version.
Dr Kashini Andrew, lead author of the study and the Specialist Registrar at University Hospitals Birmingham NHS Foundation Trust in the UK, said: ‘This study has demonstrated how AI is rapidly improving and learning, with the high accuracy directly attributable to improvements in AI training techniques and the quality of data used to train the AI.’
He added the technology has the capacity to ‘[free] up more time for patients that need urgent attention.’
When examining the skin for cancerous growths, Dermatologists follow the ABCDEs: asymmetry, border, color, diameter and evolving.
Most melanomas, the rarest but most dangerous form of skin cancer that is most likely to spread, present as asymmetrically (the ‘A’ in the ABCDEs) shaped moles that have uneven edges.
Irregular borders of a mole, the ‘B’ in ABCDEs, can also indicate melanoma. The edges of a normal mole are uniform and smooth.
A suspicious mole often contains several shades of brown, black, or tan, as well as spots of pink, red, or purple, and it becomes more colorful as cancer progresses.
Melanomas typically present a bit bigger than a pea or a pencil eraser, about six millimeters or a quarter inch in diameter.
Melanoma grows in two phases, horizontal and vertical. This represents the ‘E’ in the ABCDEs of melanoma diagnosis.
The horizontal phase can last years before the mole becomes dangerous and invasive, meaning it spreads to lymph nodes and organs. But in a later phase, the lesion grows vertically, at which point it becomes a tumor with the ability to spread elsewhere in the body, potentially proving fatal.
Non-melanoma skin cancers manifest themselves differently, often beginning as waxy or red bumps on the skin. The researchers reported having considered all other types of skin cancers, which would include those detailed below.
Merkel cell carcinoma, the type of skin cancer that killed Jimmy Buffett, is a rare and aggressive form of skin cancer. It grows quickly and often spreads to lymph nodes before ravaging other organs.
The cancer of Merkel cells, which are located in the outermost layer of the skin called the epidermis, is about 40 times more rare than melanoma. While approximately 98,000 Americans will receive a melanoma diagnosis in one year, just 3,000 people get an MCC diagnosis annually.
Yearly screening is recommended as early action is crucial. In fact, 99 percent of patients who detect and begin treating their melanoma early survive five years or more after their diagnosis.
Basal cell carcinoma, which typically appears on sun-exposed parts of the body like hands, neck, arms, and legs, often presents as a waxy lump or a small, smooth, shiny, or pale growth.
It does not always appear raised, though, and could resemble a flat scar.
Another type of non-melanoma called squamous cell carcinoma typically appears as a patch of red, scaly skin that sometimes bleeds. It can also appear as a raised scar.
People who have a history of heavy sun exposure are most likely to experience this type of skin cancer.
Of all basal cell carcinoma cases diagnosed, the AI software only missed one. But a ‘safety net’ system in which a doctor reviewed what the technology missed was able to spot the cancer.
This led researchers to include the major caveat that AI capabilities have not advanced enough that they could take the place of a practicing doctor to accurately spot problems.
Dr Irshad Zaki, Consultant Dermatologist at University Hospitals Birmingham NHS Foundation Trust and co-author of the study, said: ‘We would like to stress that AI should not be used as a standalone tool in skin cancer detection and that AI is not a substitute for Consultant Dermatologists.
‘AI is currently not a stand-alone tool in dermatology. Our data shows the great promise of AI in future provision of healthcare.’
The researchers’ findings were presented at the European Academy of Dermatology and Venereology (EADV) Congress of 2023 in Berlin.